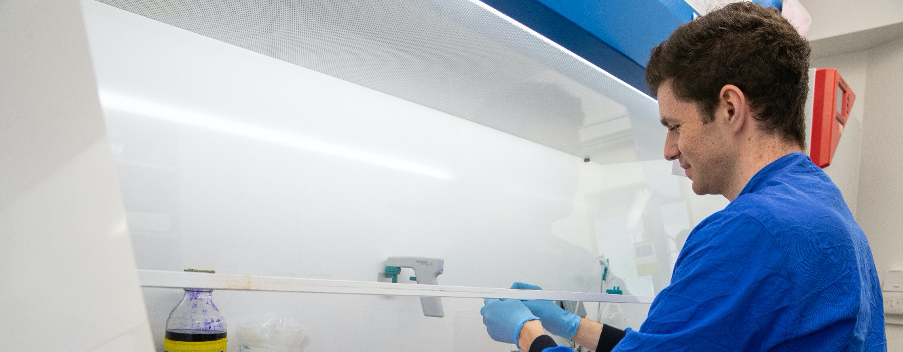
Alex Sampson (2014) is part of a Cambridge team creating a DNA vaccine to counter COVID-19. Here he shares his experience of joining the team and working on the vaccine alongside his final exams.
I started working on the COVID-19 vaccine just over six months ago. As a final year veterinary student at St John’s, I’ve always been interested in viruses and vaccines, and, in particular, the dangerous pathogens that pass from animals into humans. I’d worked on an Ebola vaccine in my 4th year summer in a Cambridge lab with Professor Jonathan Heeney, and I followed the news about the novel coronavirus closely in the early days of the pandemic. It was still a surprise to see Professor Heeney on television shortly after Italy went into lockdown, when it was clear that the UK was not far behind. He was discussing his team’s efforts to design a vaccine for COVID-19. Without stopping to think, I emailed offering to help, and within a few hours he’d invited me to visit the next morning. Other than a few weeks off for my final exams, I’ve been working on the vaccine ever since.

It was immediately clear how serious this work was: on my first day, the team was trained to keep the animal centre running so that if all the staff fell sick or were incapacitated, we could continue the trial for as long as possible. The progress the team had made in such a short period of time was remarkable — they’d already generated several sets of prototypes and identified the best candidates — but there was still a lot to do before approval for clinical trials, and the looming first wave was beginning to materialise. My main memories from this early period were cycling in on empty roads during the peak of lockdown and revising veterinary diseases for my exams in between experiments. It was bizarre to return home and see the Prime Minister discussing our work on television, and it was particularly sobering to think of vulnerable family members and friends who were then ill with COVID-19.
The SARS-CoV2 virus (the pathogen that causes COVID-19) is covered in ‘spike’ proteins, which are long extensions that grab onto our cells and allow the virus to enter. It is thought that antibodies against these spikes are our best chance at immunity against SARS-CoV2, so the goal of most vaccines is to induce anti-spike antibodies that block the virus infecting our cells. Our vaccine shares this approach, but it is unique in several ways: we have focused on the most critical part of the spike to induce only the most targeted antibodies, and we are identifying features shared by other coronaviruses besides SARS-CoV2. The technology used to deliver the vaccine is also novel: we are using DNA, rather than inactivated virus or viral proteins, and the vaccine can be dried into a powder and delivered without a needle, making it easier to distribute to regions of the world where keeping the vaccine refrigerated during transit is challenging.

When I started in March, I joined a fantastic team of dedicated, hard-working people, who had dropped everything and put their normal lives on hold in February, and who have worked tirelessly ever since. There’s a cohesive atmosphere within the team and a real sense of momentum in the project. It’s a testament to the team’s extraordinary efforts that our vaccine has been funded for Phase 1 trials in humans, due to start as soon as possible. My main role has been developing virus-like particles to use as safer substitutes of the live virus so that we can study antibody responses. I initially started making SARS-CoV2 decoys, and these have now been successfully used to test all of our vaccine designs and sent to our collaborators across the country. Lots of tests measure the total levels of antibody, and the decoys allow us to identify whether those antibodies are actually effective. Since my graduation in June, I’ve been making decoys for the other coronaviruses that infect humans and for similar coronaviruses in bats that could potentially pass into humans in the future. Our hope is that our vaccine can protect against all of these threats — not just to help combat this pandemic, but to make sure we’re prepared for any future coronaviruses.
At the same time, we’ve been part of a country-wide consortium studying how immunity to SARS-CoV2 developed in a cohort of patients infected during the first wave, and identifying any correlations in these patients with disease severity. It’s been really exciting working with this group of collaborators, some of whom have worked on coronaviruses since the 2004 SARS-1 pandemic, and the information we’ve collected has been essential to understanding which parts of the immune system are important in protecting us against disease.

The COVID-19 pandemic has changed so many aspects of our lives. In March I was just starting to prepare for my final exams and was looking forward to enjoying my last few months at St John’s with my housemates before starting work at a small animal clinic.
One of the events I was most sad to miss was my graduation with the other vets and medics at St John’s, which was meant to be a celebration for students, staff and our families after six years together. Despite this, it’s been an incredibly exciting last six months. The exhilarating pace and collaborative nature of the global effort to combat coronavirus has been unprecedented, and it has been a privilege to be involved in such important work.